Researchers cure mysterious, deadly skin disease with groundbreaking technology
Researchers from the University of Copenhagen have helped cure a life-threatening skin disease in seven patients with the help of advanced protein analysis. It marks the first time that the method is applied to treat patients, posing great potential for treating other diseases with unknown, underlying causes.
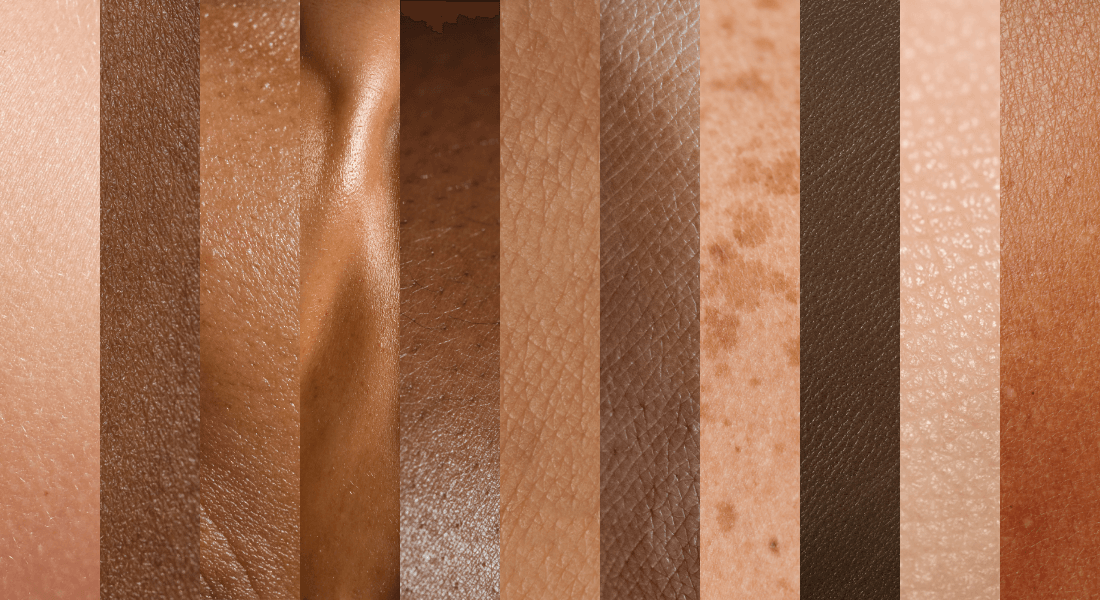
It sounds like something right out of a horror film: A devastating and lethal skin condition that causes the skin to die and fall off.
It is not fiction, however, but a very real skin disease. Toxic epidermal necrolysis, or TEN, is a rare autoimmune response, triggered by common medications, antibiotics or by a viral or bacterial infection. It has a mortality rate of 30 per cent.
Scientists have been at a loss of why it occurs and, until now, there has been no effective cure for the disease.
But with the use of an advanced analytical method pioneered at the Faculty of Health and Medical Sciences known as deep visual proteomics (DVP), researchers were able to identify the root cause of the lethal skin disease at the protein level.
Deep visual proteomics
Deep visual proteomics (DVP) is a combination of advanced tools used to study proteins and how they behave and interact.
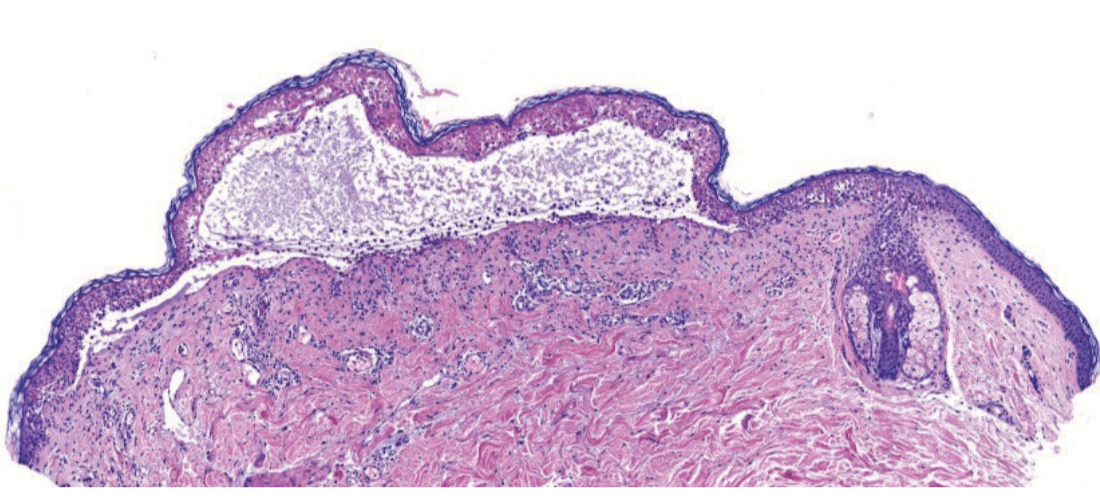
First, DVP combines high resolution microscopy and artificial intelligence to create an extremely detailed digital map of the diseased tissue by segmenting the many individual cells in the sample. Now, the researchers know where the cells are located in the sample.
Second, the researchers extract the morphology, texture and other data from the cells that look most interesting and individually cut out the relevant cells with a laser microdissection microscope.
Third step is to chemically digest the proteins in the cells into even smaller components known as peptides. The peptides are then fed to a mass spectrometer which is used to identify and quantify the thousands of proteins in the sample.
Finally, researchers can map the mass spectrometer data back onto the original digital map of the tissue sample. This enables researchers to see if anything stands out at a protein level. This knowledge can then be used to find medication that directly targets the molecular mechanisms causing the disease.
”By using this technology, we were able to show the underlying, molecular cause of TEN. To our knowledge it is the first time that spatial omics were directly used to cure patients, which is amazing. It really shows the power of this technology,” says Associate Professor Andreas Mund from the Novo Nordisk Foundation Center for Protein Research (CPR), who helped pioneer deep visual proteomics. He is part of the global team identifying the cause of TEN led by Professor Matthias Mann from CPR and the Max Planck Institute of Biochemistry (MPIB).
The discovery led researchers to treat seven TEN patients with medication that suppresses specific protein interactions in our cells. All seven patients fully recovered. This marks the first time that the advanced analytical method DVP was directly applied to patients, curing them completely.
The first ever treatment with JAK inhibitors
Simply put, DVP is a series of advanced technological methods that researchers use to analyse and map how proteins behave in their natural environment, for instance in a tissue sample from a patient with the disease. With DVP, the researchers make tiny underlying mechanisms in our proteins stand out and explain processes in our cells which are otherwise invisible to the naked eye – or even through regular microscopes.
In the case of toxic epidermal necrolysis, first author Thierry Nordmann, a dermatologist and clinician-scientist from MPIB, applied DVP to skin samples with the disease. The researchers then noticed that a specific protein interaction, known as the JAK-STAT signaling pathway, was over-active.
An international team of researchers from Germany, Australia and Japan then validated the findings in a series of pre-clinical studies.
To cure TEN, researchers would then normally need to develop medication that inhibits this specific interaction, a process that takes years. Luckily, such medication based on so-called JAK inhibitors already exists, originally developed to treat rheumatoid arthritis and eczema.
In collaboration with clinical teams, the researchers administered the safe and tested medication to the TEN patients. They all fully recovered.
“Until now, patients with TEN would get treated with a variety of other anti-inflammatory drugs to help with the inflammation, but none have proven fully effective to date. With JAK inhibitors and already after a couple of days of use of this repurposed drug, we noticed that disease progression stopped, and the skin started to heal. After using it for approximately a month, seven out of seven patients were cured”, says Thierry Nordmann.
Proteins should be primary targets for cures
The remarkable results show great potential for curing other TEN patients, and the next step for the researchers is to develop medication through clinical trials directly targeting TEN.
While larger clinical trials are needed to confirm the efficacy and safety of the repurposed medication in treating TEN, the research highlights the potential of DVP for future drug development and repurposing.
It is a very generic technology that can be applied to any kind of disease where we don’t know the underlying cause.
And the future applications are almost endless, Andreas Mund points out:
“It is a very generic technology that can be applied to any kind of disease where we don’t know the underlying cause. As long as you have a tissue sample, whether it is from the skin, the liver, the pancreas or something else, DVP could be used for it,” he says, adding:
“For example, we are currently investigating how DVP can help us better understand atherosclerosis, or for studying organ development and modeling, all kinds of liver diseases and other skin diseases like skin cancer. We can imagine many more cases like this, where deep visual proteomics could play a similar role.”
This way, DVP can be used to develop very precise medical treatments that target the underlying protein mechanisms.
“Proteins are extremely interesting. They are the functional units of the body and if you want to understand disease development and progression and find a cure for it, proteins should be the primary target. By targeting the specific proteins that cause the disease directly, you target the disease more precisely. This is a more effective method compared to medication that works more broadly,” adds Matthias Mann, corresponding author of the study.
Read the article “Spatial proteomics identifies JAKi as treatment for a lethal skin disease.”
Contact
Associate Professor Andreas Mund
andreas.mund@cpr.ku.dk
+45 35 32 50 69
Communications Consultant William Brøns Petersen
william.petersen@sund.ku.dk
+45 93 56 55 80
